 The aorta; by far one of my favorite great vessels to lay my sono-eyes on–sure, sure, it can be challenging on occasion but hey– “A challenge only becomes an obstacle when you bow to it.” ― Ray Davis
The aorta; by far one of my favorite great vessels to lay my sono-eyes on–sure, sure, it can be challenging on occasion but hey– “A challenge only becomes an obstacle when you bow to it.” ― Ray Davis
That said, there are sono-standards published by the AIUM which I will paste below; this gives an overview of what is to be included in an aortic ultrasound, but leaves a bit to be desired when talking technique; cue the sono-insight from the girl at the disposal of sono-tip seekers. At your service 😉
SAGITTAL IMAGING
When you’re scanning the aorta in sagittal, you will be obtaining AP measurements at the proximal, mid, and distal segments. The most frequent uncertainty of students–and some rads–yeah, they don’t know EVERYTHING–just don’t tell them that ;)–is where to place the calipers.
The aorta is measured from outside wall to outside wall according to AIUM standards.
It’s also a nice touch for reference, to use other vessels as landmarks along the length of the aorta when possible; this further illustrates your location for the radiologists. At the proximal segment, I will usually try to get the SMA origin. While there’s not much else, in terms of vessels arising from the anterior of the abdominal aorta, that you can ROUTINELY use as a reference point in sagittal; if you’re feeling squirrely you can try for the IMA (distal to the SMA).
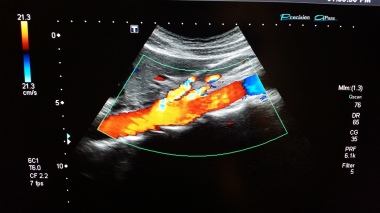
I also drop color and Doppler to get a pretty waveform if possible in each segment because I like to and I can, though most wouldn’t consider it “necessary” in a normal abdominal aorta. However; you may find that doing what isnt necessary, yet still relevant can be a way of branding yourself;though not all rads will give you accolades for it.
Now, if during your sagittal evaluation, you run into an aneurysm, you will want to get the craniocaudal length (i.e. where it starts to where it ends). You also need to capture and document any intraluminal pathology such as thrombus, calcific plaque, or dissection. Also be sure to drop color in the aneurysm to demonstrate the disturbance of flow within the greatest area of dilatation; this will also highlight areas without flow, such as mural thrombus and/or dissection, where the absence of color can indicate a false lumen. You will continue the same technique through the bifurcation and bilaterally into the proximal iliacs to get the AP dimension.

TRANSVERSE
Your transverse imaging will mirror the protocol above in the axial plane. Take your TRV measurements at the proximal (celiac trunk as a landmark), mid (renal vessels landmark) distal, and the proximal iliacs where it bifurcates. I typically drop color on the trv iliacs to highlight the vessels since they are so small and can easily be lost in the bowel gas.
AIUM: Specifics of the Aorta Sonography Examination
At a minimum, the diagnostic examination includes the following, when feasible:
- Longitudinal images of the proximal, mid, and distal abdominal aorta with anterior to posterior measurement
- Transverse images of the proximal, mid, and distal abdominal aorta
- Longitudinal images of the right and left common iliac arteries with anterior to posterior measurement
- Transverse image of the right and left common iliac arteries near the aortic bifurcation
- Color Doppler imaging and/or spectral Doppler imaging with waveform analysis, as indicated.
- Documentation of mural thrombus if present













You must be logged in to post a comment.